Everything you need to know about metabolic disorders
The current state of metabolic health
Modern lifestyles, characterized by sedentary behavior, ultra-processed foods, and refined carbohydrates, have led to a rising prevalence of metabolic health issues in recent years.
This is just a snapshot of the status quo:
- 74% of U.S. adults are overweight or obese (42.5% of U.S. adults aged 20 and over are obese, and another 31.1% are overweight) [1].
- 17% of U.S. children fall into the obese category [2].
- 52% of American adults have prediabetes or T2DM [3].
- 28% of U.S. teenagers show signs of prediabetes [4].
- 18% of U.S. teens are affected by non-alcoholic fatty liver disease (NAFLD) [5].
- 8–20% of women globally are estimated to have polycystic ovary syndrome (PCOS), a condition linked to metabolic dysfunction [6].
These statistics highlight that both metabolic syndrome and metabolic disorders are becoming more common across all age groups, indicating the need for early intervention and prevention strategies.
Metabolic syndrome vs. metabolic disorder: What’s the difference?
Metabolic syndrome refers to a cluster of interconnected risk factors that increase the likelihood of developing cardiovascular diseases, type 2 diabetes mellitus (T2DM), and other health complications [7]. It is a clinical diagnosis based on specific criteria such as abdominal adiposity, insulin resistance, hypertension, and dyslipidemia.
While metabolic syndrome is a precursor and warning sign, metabolic disorders are the outcome of prolonged metabolic dysfunction and include type 2 diabetes, obesity, and atherosclerosis.
Both metabolic syndrome and metabolic disorder represent different points on the spectrum of metabolic health challenges and often result from or contribute to metabolic inflexibility—the diminished ability of mitochondria, your cells’ powerhouses, to efficiently switch between burning carbs and fats for energy.
A closer look at metabolic syndrome
Metabolic syndrome is when an individual has at least three of the following risk factors:
- Abdominal adiposity
- Excess fat around the waist (measured by waist circumference) is a hallmark of metabolic syndrome. Visceral fat, in particular, is strongly linked to insulin resistance and inflammation [8].
- Insulin resistance
- Insulin resistance occurs when your cells become less responsive to insulin, leading to elevated blood glucose levels. This is a precursor to type 2 diabetes [9].
- Hypertension (HTN)
- High blood pressure is a common feature of metabolic syndrome, increasing the risk of cardiovascular complications.
- Dyslipidemia
Dyslipidemia includes abnormal cholesterol and lipid levels, such as:
- Hypertriglyceridemia: High levels of triglycerides in the blood.
- Hypercholesterolemia: Elevated total cholesterol levels.
- Low HDL: Low levels of high-density lipoprotein.
Each of these factors may have negative health consequences, but together, they significantly increase the risk of metabolic disorders and other health complications.
A closer look at metabolic disorders
Metabolic disorders are chronic conditions that result from prolonged metabolic dysfunction. Some of the most common include:
- Type 2 diabetes (T2DM)
- T2DM, characterized by persistent high blood sugar due to insulin resistance or reduced insulin production, is a major metabolic disorder affecting millions worldwide.
- Obesity
- Obesity is a risk factor for and a result of metabolic dysfunction [7]. It contributes to systemic inflammation, insulin resistance, and other health complications.
- Atherosclerosis
- A condition where plaque builds up in arteries, atherosclerosis is linked to dyslipidemia and increases the risk of heart attacks and strokes.
- Advanced cardiometabolic disease
- Cardiometabolic disease includes conditions such as heart attacks, strokes, and non-alcoholic fatty liver disease (NAFLD), all of which arise from metabolic dysfunction [10].
These disorders highlight the consequences of poor metabolic health and underscore the importance of early detection and prevention.
The spectrum of metabolic flexibility and inflexibility
Metabolic syndrome and metabolic disorders are closely interlinked with metabolic health and flexibility.
Metabolic flexibility refers to the body’s ability to efficiently switch between using carbohydrates and fats for energy depending on their availability and the body’s energy demands.
When you’re metabolically flexible, you can more easily lose weight, burn fat, process carbs, and improve your body composition.
Metabolic inflexibility, on the other hand, is associated with insulin resistance, reduced fatty acid oxidation, T2DM, and obesity [11]. Signs of metabolic inflexibility include:
- Difficulty managing weight
- Insulin resistance
- Increased cravings
- Persistent fatigue

The importance of metabolic tracking and lifestyle strategies for metabolic disease prevention
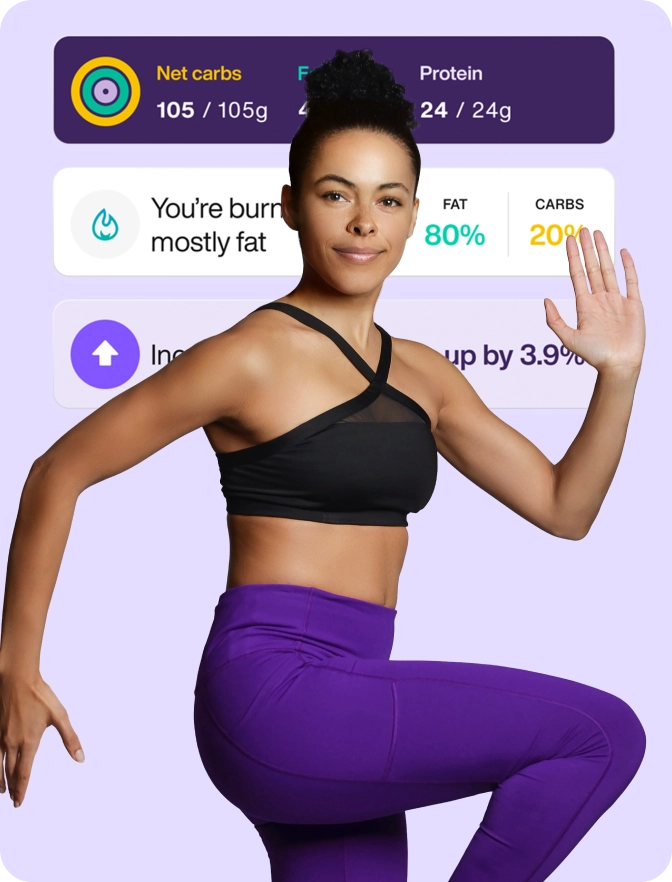
Measuring your metabolism and improving your metabolic flexibility through lifestyle adjustments can help prevent metabolic syndrome and metabolic disorders.
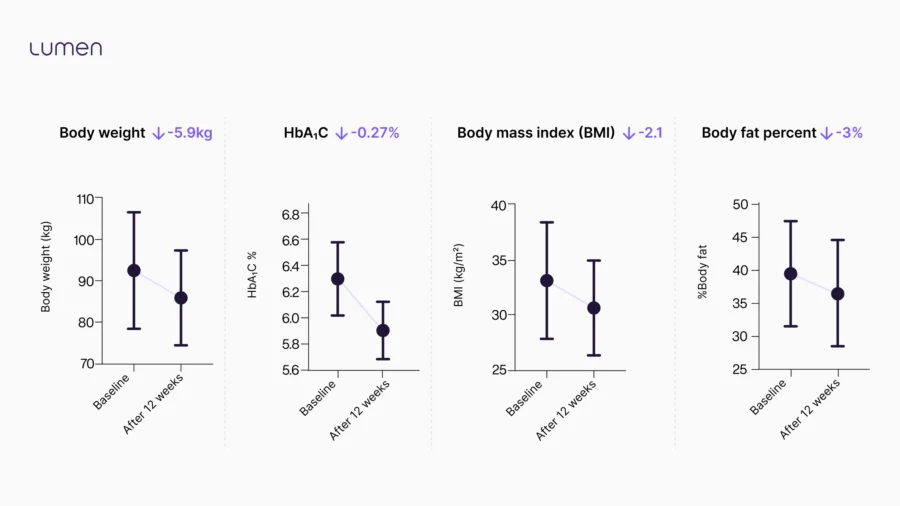
In a 12-week study including 27 prediabetic participants with a high BMI, patients using Lumen experienced changes in critical prediabetic health markers [12].
Participants followed nutritional and lifestyle recommendations given by Lumen based on their metabolic measurements. Prediabetics who used Lumen for 90 days saw a significant reduction in four key metabolic health indicators:
- 5.9 kg reduction in body weight
- 0.27% lower hemoglobin A1c
- BMI reduced by 2.1 points
- 3% lower body fat percentage
This indicates that understanding how your body responds to your lifestyle is a powerful tool for improving your health. Let’s take a closer look at how.
“Metabolic flexibility is important for better overall health, better stress management, and feeling more energized and less sluggish.”
Dr. Caroline Leaf, Clinical Neuroscientist
Measure your wake-up breath: Do you spot short- and long-term trends?
Using a metabolic tracker to measure your metabolism upon waking is a great way to gauge your mitochondrial state and metabolic health. It provides valuable insights into how your lifestyle is affecting you in the short and long term.
Waking up in fat burn is the goal and means your mitochondria are efficient since fat is the ideal fuel during rest and fasting. If you wake up in carb burn once in a while, short-term causes could be a late-night meal, eating carbs later in the day, or illness.
If you consistently wake up in carb burn, it may be an early indicator of metabolic syndrome. It can suggest that your body is not efficiently utilizing fat for energy, signaling the need to adjust your lifestyle choices—whether nutrition, fitness, sleep, or stress management.
Measure your metabolism pre- and post-meal: Is there a shift?
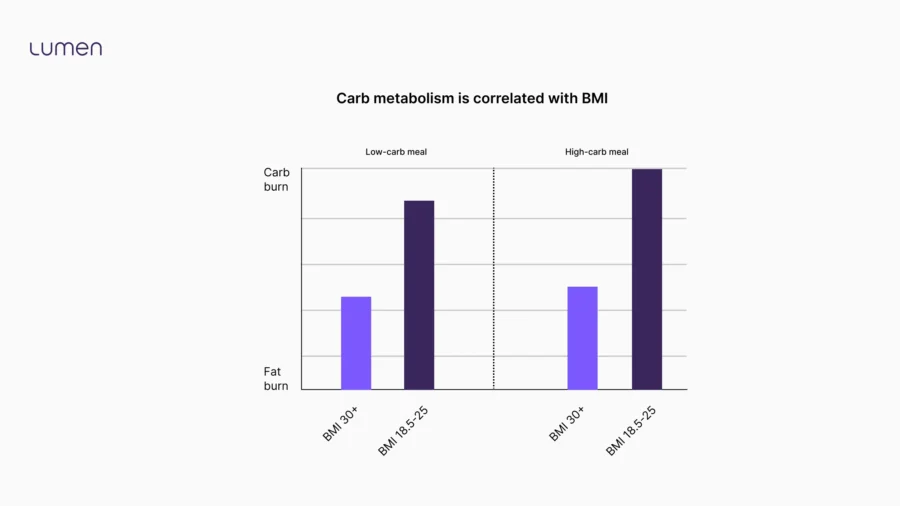
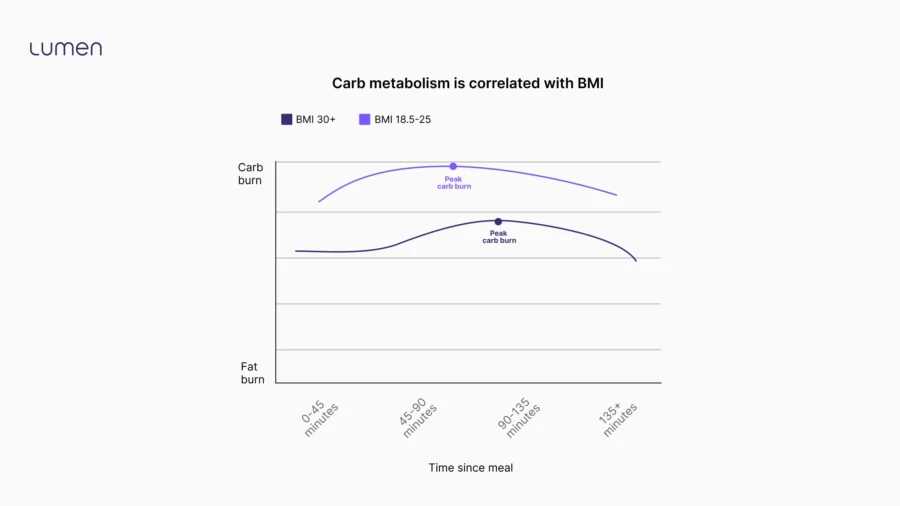
To gauge how your body responds to the food you eat, measure your metabolism before and after a carb-rich meal to see if your mitochondria shift to burning carbs. In a retrospective study by Lumen with 2,607 participants, people with a healthy BMI and better metabolic flexibility demonstrated a greater post-meal carb response, burning more of the carbs they ate for energy rather than storing them as fat [13].
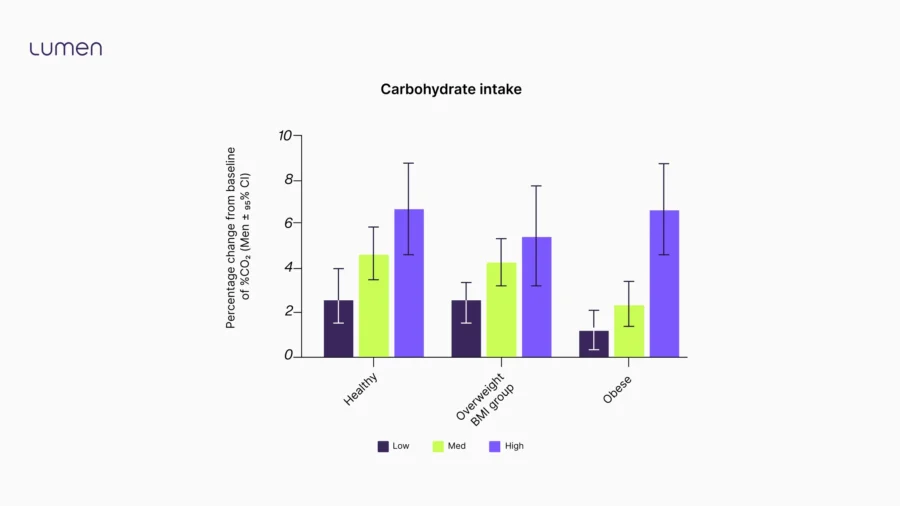
This aligns with results from our latest Lumen Experiments, involving 2,700 Lumen community members, which showed that participants with a BMI of 18.5–25 demonstrated:
- A faster and stronger carb response after eating. This means they are more likely to use the carbs they eat for energy rather than store them as fat.
- Higher CO2 levels even 2+ hours after eating, indicating more metabolic activity.
What does this mean for you?
When you improve your metabolic flexibility, you can:
- Enjoy carbs without the risk of weight gain
- Use the carbs you eat for energy to keep you fueled
- Indulge occasionally, knowing your metabolism can handle the extra carbs
Build up your muscle mass and maintain it: Take a pre-workout metabolic measurement
Your muscles are packed with mitochondria and house most of your glycogen. This means the more muscle mass you gain, the more mitochondria and glycogen stores you’ll have. As a result, your muscles can efficiently use carbs when you need an energy boost, ensuring less glucose is stored as fat. It also helps your mitochondria better metabolize fat at rest or during low-intensity activities.
To maintain your hard-earned muscle mass, measure your metabolism before a high-intensity workout to ensure you have enough carbs to support your exercise and prevent muscle breakdown. If you’re burning fat before your high-intensity workout, that’s a sign to eat some healthy, fast-digesting carbs before you begin exercising.
Mind your carbs for insulin sensitivity and glycogen balance
Shifting between carbohydrate and fat metabolism depends on key physiological mediators such as glycogen, your body’s form of carb storage found in the muscles and liver, and insulin sensitivity. These mediators are influenced by various factors, including the quantity, type, and timing of carbs you consume.
A metabolic tracker can help you determine how many carbs to eat, which kinds, and when based on your metabolic measurements.
Why the amount of carbs you eat matters
Eating a balanced ratio of complex carbs, healthy fats, and quality protein prevents an over-reliance on carbs for energy, which helps manage blood glucose levels and glycogen.
Eating more carbs than you can store as glycogen forces your body to convert the excess into fat [9]. At the same time, this overworks your mitochondria, causing oxidative stress that damages their membranes. Plus, chronically high glycogen levels can make your mitochondria overly reliant on carbs and reduce their ability to burn fat effectively, hampering weight loss and body recomposition efforts.
When fat cells become hypertrophied due to excess fat storage, they attract macrophages that release proinflammatory cytokines, such as IL-6 and TNF-α. Encouraging fat burn and improving insulin sensitivity helps reduce the infiltration of these inflammatory cells, lowering systemic inflammation and decreasing the risk of type 2 diabetes, cardiovascular diseases, and certain cancers [14].
When your glycogen stores are just full enough, they can fuel your mitochondria quickly to provide energy boosts as needed, such as when weightlifting or sprinting [15].
Alternating between high-carb and low-carb days based on your metabolic measurements will help to deplete and replenish your glycogen and encourage your mitochondria to shift between carb and fat burn.
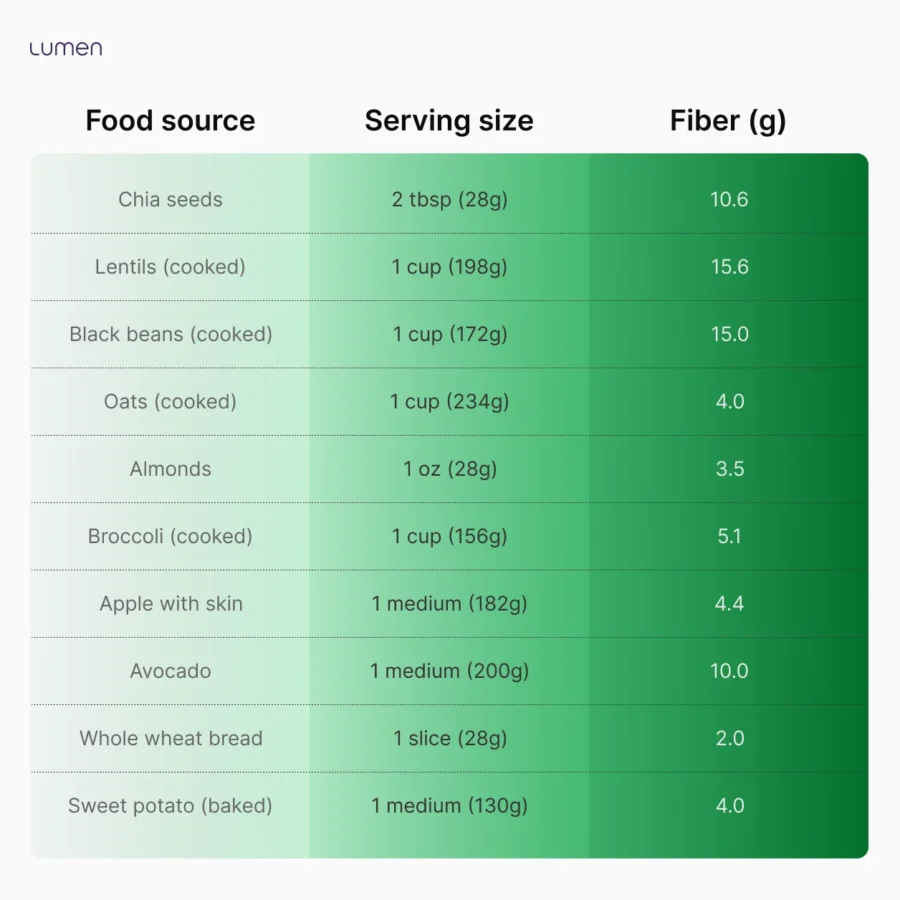
Understanding the role of complex carbs
The type of carbohydrates you consume can play a critical role in metabolism. Complex carbohydrates, such as whole grains, legumes, and vegetables, provide a steady release of glucose into the bloodstream, helping maintain blood glucose stability, enhance insulin sensitivity, and reduce cravings. High insulin sensitivity means your body needs only a small amount of insulin to help glucose reach your mitochondria and support energy production for daily activities.
Because simple carbohydrates don’t contain as much fiber as complex carbs, they can cause rapid spikes in blood sugar and insulin [16], leading to energy crashes and increased hunger.
Fiber is a type of carbohydrate that the body cannot digest. Unlike other carbohydrates, such as sugars and starches, fiber passes through the digestive system relatively intact.
Soluble fiber forms a gel-like substance in the gastrointestinal tract, slowing the digestion and absorption of carbs. This gradual release of glucose into the bloodstream prevents sharp spikes in blood sugar and therefore insulin levels, helping to prevent insulin wear-out and insulin resistance.
Certain fibers serve as food for beneficial gut bacteria and can enhance insulin sensitivity by reducing systemic inflammation.
Why carb timing is essential
Food timing can significantly impact your metabolism. Research shows that eating carbohydrates earlier in the day aligns with the body’s natural insulin sensitivity peaks, supporting efficient glucose metabolism [17].
On the other hand, consuming high-carb meals later in the evening can hinder the overnight shift to fat burn, potentially impairing sleep quality. Eating an earlier dinner also supports mitochondrial function, allowing a more effective transition to fat burn during sleep. Timing carbohydrates around exercise is another effective strategy to boost metabolism. You’re more insulin sensitive post-workout, and the carbs you eat can promote glycogen replenishment, recovery, and building muscle mass [18]. When insulin sensitivity is high, your cells can efficiently absorb glucose from the bloodstream and use it for energy. Moreover, improved insulin sensitivity ensures the body can efficiently convert glucose into glycogen rather than fat.
Your metabolism is flexible: Make the changes that matter for long-term health
Metabolic syndrome and metabolic disorders are intricately connected. Understanding these conditions and recognizing their early signs can empower individuals to take proactive steps toward improving their metabolic health.
Promoting metabolic flexibility through targeted lifestyle changes may decrease your risk of metabolic syndrome and related disorders. Given the current statistics, improving metabolic health is essential.
Proactive measures today can lead to a healthier future, mitigating the burden of metabolic dysfunction and its related complications.
Sources
[1] Fryar, C. D., Carroll, M. D., & Afful, J. (2020). Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health E-Stats.
[2] Sanyaolu, A., Okorie, C., Qi, X., Locke, J., & Rehman, S. (2019). Childhood and Adolescent Obesity in the United States: A Public Health Concern. Global pediatric health, 6, 2333794X19891305. https://doi.org/10.1177/2333794X19891305
[3] Menke, A., Casagrande, S., Geiss, L., & Cowie, C. C. (2015). Prevalence of and Trends in Diabetes Among Adults in the United States, 1988-2012. JAMA, 314(10), 1021–1029. https://doi.org/10.1001/jama.2015.10029
[4] Liu, J., Li, Y., Zhang, D., Yi, S. S., & Liu, J. (2022). Trends in Prediabetes Among Youths in the US From 1999 Through 2018. JAMA pediatrics, 176(6), 608–611. https://doi.org/10.1001/jamapediatrics.2022.0077
[5] Arshad, T., Paik, J. M., Biswas, R., Alqahtani, S. A., Henry, L., & Younossi, Z. M. (2021). Nonalcoholic Fatty Liver Disease Prevalence Trends Among Adolescents and Young Adults in the United States, 2007-2016. Hepatology communications, 5(10), 1676–1688. https://doi.org/10.1002/hep4.1760
[6] Singh, S., Pal, N., Shubham, S., Sarma, D. K., Verma, V., Marotta, F., & Kumar, M. (2023). Polycystic Ovary Syndrome: Etiology, Current Management, and Future Therapeutics. Journal of clinical medicine, 12(4), 1454. https://doi.org/10.3390/jcm12041454
[7] Swarup, S. (2024, March 7). Metabolic syndrome. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459248/
[8] Hardy, O. T., Czech, M. P., & Corvera, S. (2012). What causes the insulin resistance underlying obesity?. Current opinion in endocrinology, diabetes, and obesity, 19(2), 81–87. https://doi.org/10.1097/MED.0b013e3283514e13
[9] Freeman, A. M. (2023, August 17). Insulin resistance. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK507839/
[10] Khan, A. R., Salama, A. H., Aleem, Z., Alfakeer, H., Alnemr, L., & Shareef, A. M. M. (2023). The Promising Frontier of Cardiometabolic Syndrome: A New Paradigm in Cardiology. Cureus, 15(9), e45542. https://doi.org/10.7759/cureus.45542
[11] Goodpaster, B. H., & Sparks, L. M. (2017). Metabolic Flexibility in Health and Disease. Cell metabolism, 25(5), 1027–1036. https://doi.org/10.1016/j.cmet.2017.04.015
[12] Buch, A., Yeshurun, S., Cramer, T., Baumann, A., Sencelsky, Y., Zelber Sagi, S., Serebro, M., Greenman, Y., Mor, M., & Eldor, R. (2023). The Effects of Metabolism Tracker Device (Lumen) Usage on Metabolic Control in Adults with Prediabetes: Pilot Clinical Trial. Obesity facts, 16(1), 53–61. https://doi.org/10.1159/000527227
[13] Yeshurun, S., Cramer, T., Souroujon, D., & Mor, M. (2024a). The Association of Macronutrient consumption and BMI to exhaled carbon dioxide in lumen users: Retrospective real-world study. JMIR mHealth and uHealth, 12. https://doi.org/10.2196/56083
[14] Song, D. K., & Kim, Y. W. (2023). Beneficial effects of intermittent fasting: a narrative review. Journal of Yeungnam medical science, 40(1), 4–11. https://doi.org/10.12701/jyms.2022.00010
[15] Jensen, J., Rustad, P. I., Kolnes, A. J., & Lai, Y. C. (2011). The role of skeletal muscle glycogen breakdown for regulation of insulin sensitivity by exercise. Frontiers in physiology, 2, 112. https://doi.org/10.3389/fphys.2011.00112
[16] Holesh, J. E. (2023, May 12). Physiology, carbohydrates. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459280/
[17] Lopez-Minguez, J., Gómez-Abellán, P., & Garaulet, M. (2019). Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk. Nutrients, 11(11), 2624. https://doi.org/10.3390/nu11112624 Kerksick, C. M., Arent, S.,
[18] Schoenfeld, B. J., Stout, J. R., Campbell, B., Wilborn, C. D., Taylor, L., Kalman, D., Smith-Ryan, A. E., Kreider, R. B., Willoughby, D., Arciero, P. J., VanDusseldorp, T. A., Ormsbee, M. J., Wildman, R., Greenwood, M., Ziegenfuss, T. N., Aragon, A. A., & Antonio, J. (2017). International society of sports nutrition position stand: nutrient timing. Journal of the International Society of Sports Nutrition, 14, 33. https://doi.org/10.1186/s12970-017-0189-4






 Digital download
Digital download